Capital Caring Health Palliative Care Nurse Brings Comfort to a Patient and his Family

Families of patients with the highly contagious COVID-19 bear a huge emotional toll, as they are unable to be near a loved one who has contracted the virus. For those needing hospitalization, the situation is even more isolating. Family members are not allowed to visit—to hold a hand, to offer reassurance with words and the sound of their voice, or even to see how their loved one looks.
For the large Kunihiro family—three adult children and grandchildren—that’s where Capital Caring Health’s Steve Skobel, a palliative care nurse practitioner, made an enormous difference. As the liaison in the hospital between seriously ill patients and families, Steve became the family’s eyes, ears and even mouth, serving as an important link between the two.
Symptoms Develop, Emergency Room Follows
Ron is a fairly active guy for his age. He works out regularly on his recumbent bike and plays golf. In early March, he developed a fever—but felt fine—until about five days later when he became slightly short of breath after minor exertion. However, as Ron was unable to be tested for possible coronavirus, he quarantined at home in the basement to protect Sue, his wife of 55 years. When he developed a wet cough, his doctor recommended—via a telehealth visit—that Ron stay at home and take a course of antibiotics for bronchitis.
But nearly a week after the fever, Ron felt worse.
In a video call with daughter Cindi Harkes, Ron was coughing and short of breath. They discussed his going to the emergency room, Ron’s doctor agreed and suggested he drive himself to the local hospital which he did the next day. Once there, Ron was intubated, placed on a ventilator and transferred to the ICU at Prince William Medical Center in Manassas, Virginia.
It would be close to four weeks before Ron would actually speak to his family again.
New Knowledge, New Approaches
Ron was, in fact, among the first one or two COVID-19 patients at the Prince William Medical Center. And in those early days of March, doctors everywhere were still trying to understand coronavirus and the most effective treatments. With double pneumonia and not expected to survive, Ron was placed in a medically-induced coma. His family—deeply religious—started making arrangements for last rites.
Instead, as understanding of the coronavirus evolved, so did treatment. On Day 13, Ron was placed in a prone position—on his stomach—and he started to improve a little. A week earlier, Steve Skobel, N.P., entered the picture.

Improved Communication
As Ron’s nurse practitioner, Steve helped establish goals for his patient and saw him every day. Soon he was holding daily conference calls with the family after he had a chance to see Ron and review his chart. Ron’s daughter-in-law Amy Kunihiro—a California-based physician—often spoke or texted Steve before the calls, asking the questions which were on all of their minds.
“When I talk to families, I spend a lot of time listening to their concerns, what their needs are, what they are asking me for,” says Steve. Because he “met” with the family daily, he was able to anticipate what information they wanted and also to build rapport.
“It was so helpful that Steve was able to break down clinical information into understandable, digestible bits for everyone,” Amy says. “As a physician, I also appreciated having a dialogue with another healthcare professional about evolving treatment and recommendations based upon experiences in Italy and New York.”
Knowing they had a dedicated healthcare contact on site brought Ron’s family great relief.
“The daily calls were a ‘lifeline,” Amy continues, “adding important details on how Ron was doing, even when the news was not good. Steve would tell us ’Dad looks good today’ which was detailed description we desperately needed because we couldn’t see or hear him.
He also provided medical updates, forwarded questions and, most importantly for Cindi, “conveyed to dad the things we could not say in person.”
Despite the initial improvement from being repositioned, however, Ron experienced serious setbacks along the way, including dropping oxygen levels.
“The whole healthcare team latched on to Ron,” says Steve. “He was bed-bound for almost two months. There were many times, many days that I didn’t think he would survive to the next morning.”
But thanks to great care, faith, and his own resilience, Ron eventually began to improve. As he was brought out of the medically-induced coma, Ron flashed a thumbs-up sign to Steve and he was moved to an acute-care unit to continue regaining this health.
A Turn for the Better, Then Home
On Day 42, Ron was finally discharged from the hospital. But there was one more stop before heading home: an inpatient rehab facility. Anyone who has been in an ICU and on a ventilator as long as Ron usually experiences serious consequences. And with the COVID-19 diagnosis, supplemental oxygen is also often on the list. As a result, most patients can expect a long stay in rehab for physical and occupational therapy to help with activities like swallowing, and speech therapy. Not so for Ron—he was discharged after only 8 days.
Now after four weeks of home health care, Ron is walking independently—only using a cane for support—and is back to riding his recumbent bike. “He’s trying to get back to normal” says Cindi. “It’s truly amazing the progress he has made from where he was.”
“It was our good fortune—and Ron’s—that nurse practitioner and our liaison was Steve,” says Amy. “He’s an outstanding nurse practitioner and human being, compassionate and in a class by himself.”
Adds Cindi, “Having a liaison or advocate is invaluable to the well-being of patients and families as communication can be difficult. And as in the best communications, it goes both ways. Don’t be afraid to ask questions.”
Steve, in turn, praises the family for their close involvement in Ron’s care and recovery.
“I chose nursing because I wanted to help people,” Steve concludes “and Ron was a very, very sick man. I’m so grateful I was able to help not only him, but his entire extended family through their shared ordeal. The Kunihiros are truly thoughtful, wonderful people.”
To learn more about palliative care, hospice and elder services, visit Capital Caring Health or call (800) 869-2136.

 Kathleen Ramkaran, RN, CCM
Kathleen Ramkaran, RN, CCM Hali Gantumur
Hali Gantumur Yasmin
Yasmin  Jennifer Olsen GNP-BC
Jennifer Olsen GNP-BC Dr. Cheryl-Lynne McCalla, DO
Dr. Cheryl-Lynne McCalla, DO Meena Raj, MD,
Meena Raj, MD,  Catherine McGrady, RN, MSN, is Vice President, Clinical Programs at Capital Caring Health. In this role she is responsible for the development, implementation, and monitoring of clinical programs in support of high-quality patient-centered care delivery across the continuum of services. Catherine also manages external partnerships including Capital Caring Health’s participation in ACOs and other value-based clinical programs
Catherine McGrady, RN, MSN, is Vice President, Clinical Programs at Capital Caring Health. In this role she is responsible for the development, implementation, and monitoring of clinical programs in support of high-quality patient-centered care delivery across the continuum of services. Catherine also manages external partnerships including Capital Caring Health’s participation in ACOs and other value-based clinical programs Catherine Kravolec
Catherine Kravolec Sherri Parker
Sherri Parker Anne Young
Anne Young Odessa Simpson
Odessa Simpson Hope Collazo
Hope Collazo LaWanda Middleton
LaWanda Middleton Sally Hughes
Sally Hughes Jennifer Godwin
Jennifer Godwin Henry Fuller
Henry Fuller Margaret Doherty
Margaret Doherty Evan Kirschner
Evan Kirschner Gabby True
Gabby True Carla Thompson
Carla Thompson Shannon Collier
Shannon Collier Annette Lindsay
Annette Lindsay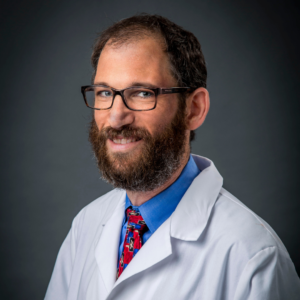 Jason Sobel, MD
Jason Sobel, MD Brenan Nierman
Brenan Nierman Susan Roberts
Susan Roberts Jackie Gouline
Jackie Gouline Stacy Brown
Stacy Brown Kremena Bikov
Kremena Bikov


 Audrey Easaw
Audrey Easaw
 Julia Feldman
Julia Feldman Gus has been a part of the Capital Caring Health family for nearly fifteen years. Ten of those years have been in leadership, working with colleagues and co-workers to achieve the best in their ability while promoting CCH core values. Gus has a background in nursing and a lifelong passion for technology. In each position at CCH, Gus has found ways to integrate technology to enhance outcomes and job satisfaction.
Gus has been a part of the Capital Caring Health family for nearly fifteen years. Ten of those years have been in leadership, working with colleagues and co-workers to achieve the best in their ability while promoting CCH core values. Gus has a background in nursing and a lifelong passion for technology. In each position at CCH, Gus has found ways to integrate technology to enhance outcomes and job satisfaction. Pat Bishop
Pat Bishop Elizabeth Ariemma
Elizabeth Ariemma Joe Murray
Joe Murray

 Lin Maurano
Lin Maurano Dwayne Barton, NP
Dwayne Barton, NP Jacob Phillips, MD
Jacob Phillips, MD Tabitha Gingerich, NP
Tabitha Gingerich, NP Donna Smith
Donna Smith Paulette Davidson, Chaplain
Paulette Davidson, Chaplain Colleen Carberry, RN Case Manager
Colleen Carberry, RN Case Manager Sherri Parker, Team Leader Medical Social Worker
Sherri Parker, Team Leader Medical Social Worker Steven Skobel’s Story
Steven Skobel’s Story Marrygold Ugorji’s Story
Marrygold Ugorji’s Story Sulaiman Bangura’s Story
Sulaiman Bangura’s Story Neil Parker’s Story
Neil Parker’s Story Michael Toohig’s Story
Michael Toohig’s Story Liberating Europe
Liberating Europe Hershell Foster
Hershell Foster Hank Willner, M.D.
Hank Willner, M.D. Laura Branker
Laura Branker Jason Parsons
Jason Parsons Altonia Garrett
Altonia Garrett
 Kieran Shah
Kieran Shah Mandy Brouillard
Mandy Brouillard
 Sherri Parker
Sherri Parker Sayaka Hanada
Sayaka Hanada Caitlin Geary
Caitlin Geary Heidi Young
Heidi Young Linda Biedrzycki
Linda Biedrzycki Heidi Young, M.D.
Heidi Young, M.D. Jason Sobel, M.D.
Jason Sobel, M.D. Anne Silao-Solomon, M.D.
Anne Silao-Solomon, M.D.

 Mohammad Saleem, M.D.
Mohammad Saleem, M.D. Maleeha Ruhi, M.D.
Maleeha Ruhi, M.D. Christopher Pile, M.D.
Christopher Pile, M.D. Cameron Muir, M.D.
Cameron Muir, M.D. Fellowship
Fellowship John McCue, D.O.
John McCue, D.O. Peyman Mamdouhi, D.O.
Peyman Mamdouhi, D.O. Adam Knudson, M.D.
Adam Knudson, M.D. Amanda Keerbs, M.D.
Amanda Keerbs, M.D. Matthew Irwin, M.D., M.S.W.
Matthew Irwin, M.D., M.S.W. Alan Goldblatt, M.D.
Alan Goldblatt, M.D. Jennifer Gerhard, D.O.
Jennifer Gerhard, D.O. Ray Jay Garcia, M.D.
Ray Jay Garcia, M.D. Tamara Barnes, M.D.
Tamara Barnes, M.D. Petros
Petros  Shaz Anwar, D.O.
Shaz Anwar, D.O. Lee-Anne West, M.D.
Lee-Anne West, M.D.
 Melissa McClean, N.P.
Melissa McClean, N.P. Michael Byas-Smith, M.D.
Michael Byas-Smith, M.D. Nancy Cook
Nancy Cook Kimberly Grove
Kimberly Grove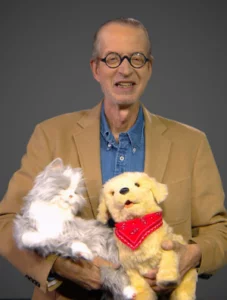 Steve Cone
Steve Cone Eric De Jonge, M.D.
Eric De Jonge, M.D. David Schwind
David Schwind Vivian Hsia-Davis
Vivian Hsia-Davis Cameron Muir, M.D.
Cameron Muir, M.D. Keith Everett
Keith Everett Susan Boris
Susan Boris Carolyn Richar
Carolyn Richar Matt Kestenbaum
Matt Kestenbaum